|
|
|
Results:
From April 1985 to November 1994, the mechanical removal of sialoliths was successful in 7 patients with sialolithiasis: 5 with submandibular duct calculi (See Figure 1 below) and 2 with parotid duct calculi (See Figure 2 below). Four patients underwent successful sialodochoplasties, 2 for parotid ducts and 2 for submandibular ducts. One patient had sialoliths and a stricture, so the total number of successful procedures was 11.
In 1 patient, the calculus was located close to the papilla, making retrieval especially difficult because of impaction. A grasping forceps was successfully used and a wide papillotomy was unnecessary.
In 2 patients, calculus retrieval failed: 1 each from the Stensen and Wharton ducts. These were technical failures caused by large impacted calculi and by strictures in the distal segment of the ducts, which made mechanical manipulation impossible. There were no sialodochoplasty failures.
The long-term outcomes following the procedures were excellent. No patient returned with recurrent symptoms. Seven patients remained symptom-free after clinical follow-up from 10 months to 10 years, and 3 patients were symptom-free for 3 to 5 years and then were unavailable for follow-up.
|
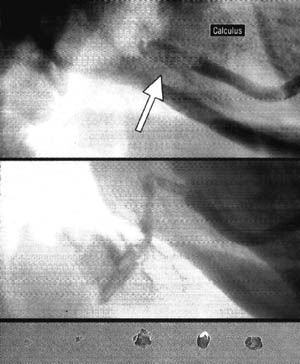
Top, Mulitple calculi are impacted in the proximal Wharton duct (arrow). Only a small amount of the contrast passes to the hilum of the gland. Center, Sialogram after basket removal of the calculi shows no residue. The round lucency in the proximal duct is introduced gas. Bottom, Five extracted calculi. These calculi are less than 3mm in diameter.
|
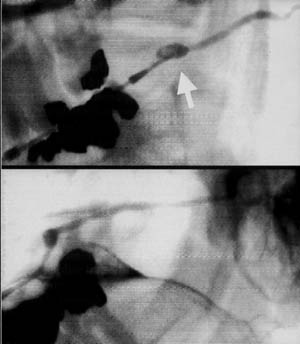
Top, Calculus in the distal segment of the partoid duct (arrow). Bottom, Sialogram after removal of the calculus with basket and grasping forceps shows small residue in the distal duct. This remaining calculus was fragmented and excreted spontaneously the next day.
|
Materials and Methods:
Before the examination, the details of the procedure and its benefits and complications were explained to the patient. Informed consent was obtained for the sialography and for the mechanical removal of the calculi, sialodocholoplasty, or both.
As an initial diagnostic examination, sialography was performed to confirm the location of the strictures and calculi. The papillae were locally anesthetized by direct injection of 1% lidocaine hydrochloride. The papillotomy was accomplished by an incision toward the duct. No sedation or general anesthesia was given.
For the removal of the calculi, a 3.5F 4-wire Dormia basket (Porges, Paliseau Cedex, Salat, France), 3F Segura basket (Microvasive Co [Boston Scientific Corp.], Watertown Mass), and 3F Coaxial Sheath Grasping Forceps (Cook Urological Co, Spencer, Ind) were used. For the sialodochoplasty, 3.8F 3-mm diameter Balloon catheters (Meditech, Watertown, Mass) were used.
After the papillotomy was accomplished, the papilla and adjacent salivary ducts were dilated by 3F and 4F dilators or stiff catheters of the same size. A 0.45-mm guide wire was introduced routinely to guide the balloon catheter. If there was a stricture, balloon dilatation was performed several times until full dilatation was achieved.
For the calculi, a basket was placed beyond or at the calculi site and the basket was manipulated to achieve extraction. When several calculi are present, several attempts may be required.
Click here to continue on to page 3.
|
|
|